Information for Healthcare Professionals
PHEM Feedback is a collaboration between a collection of acute hospital trusts, East of England Ambulance Service Trust (EEAST) and Essex and Herts Air Ambulance Trust. BASICS providers with an honorary contract with EEAST are also eligible.
It started as a twelve-month pilot which ran until April 2019. This demonstrated excellent results and we have support to continue this project until at least 2025.
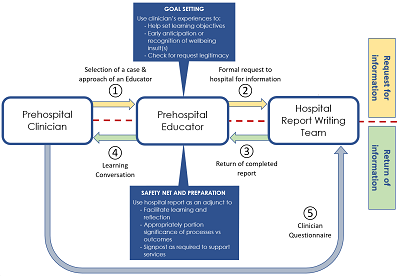
If you have a case which was challenging, you have attempted to read up to answer your query and you've approached an approved PHEM Feedback Facilitator or your HEMS Patient Liaison Manager who still can't resolve your query then they can send us a request on your behalf as long as it meets at least one of the following criteria:
- Diagnostic uncertainty. This includes:
- The range of reasonable differential diagnoses made by the clinician have conflicting management strategies that may potentially lead to harm or lack of efficacy with respect to achieving the treatment goal(s), and/or
- No reasonably accurate diagnosis can be made for reasons including rarity of the clinical features or atypical nature of the presentation and/or
- Destination hospital decision was difficult to make, such as whether or not to take a person to a tertiary stroke, trauma or heart attack centre
- Relates to critically unwell patients such as those attended by Air Ambulance organisations, those with polytrauma, those in cardiac arrest or peri-arrest etc.
- The case has had an emotional impact on the clinician which is adversely affecting professional performance, ability to rest, mental health or as otherwise determined by the senior, debriefing prehospital staff member
What you can expect from us:
- Our aim is to complete reports based on the learning objectives cited on requests in less than 2 weeks
- EEAST staff will only be provided the ED or hospital discharge diagnosis as standard but we aspire to provide more information in order to help achieve your learning objectives and do so wherever resources allow.
- Air ambulance staff can expect to get a more detailed report due to the relatively low frequency of patients admitted each month.
What we expect from you:
Please note that these documents are due for review in Spring 2021
- Read and adhere to the Terms of Service to PHEM feedback
- Respect that this is confidential information and must be treated accordingly
- To try and resolve your query through your own self-directed learning and subsequently discussion a facilitator, prior to a request being generated.
- Understanding that the PHEM Feedback team, at present, are volunteers who are fulfilling their roles in the interests of interdisciplinary working and medical education.
- Timely feedback from you to us within one week of the learning conversation with your facilitator
- Failure to return your questionnaires will risk your being excluded from accessing this service in the future so please return it for every case
Why do we need to return the questionnaires?
The success of the project and its likelihood of being available at other sites rests on us having honest feedback (even if it is constructively negative) from which we can evaluate and improve the project. The Hospital Teams go to great time and effort to provide this service so failure to reciprocate by completing the questionnaire may result in the clinician who attended the patient being ineligible for the project in the future. Similarly, we need to know if there are significant issues meeting with the facilitators in order to facilitate a solution or, in the event of multiple or ongoing concerns, escalate to more senior figures within the relevant employing organisation.
When these questionnaires are analysed we anonymise them in order to maintain the trust of our users and ensure they can reflect and raise concerns honestly and constructively without fear of those personal comments being used against them. We anonymise clinicians’ concerns raised regarding facilitators and the authors of hospital reports.
Will I risk disciplinary procedures if it turns out I made a mistake and this comes to light after my request is processed?
The PHEM feedback project will help feed into themes and trends for learning throughout the Trust. After you have received your feedback, if you are concerned that your clinical practice could have / did lead to any patient harm / potential patient harm, we would encourage you to raise an incident via your Trust’s internal reporting system. An incident review will constructively highlight areas where practice can be improved
Any incidents where a mistake has been made are dealt with fairly and within a just culture. The sole purpose of incident investigation is to learn from the incident and prevent a recurrence. This helps the Trust to enhance wider learning and ensure they do not repeat the same mistakes. Any errors in clinical care are rarely just an individual error, they are most likely part of a wider issues that can be examined. Disciplinary procedures are only brought into any incident where there is a conduct issues and this is managed through a separate HR process.
Mistakes are a part of healthcare and a core aim of our project is to help our colleagues improve the standards of care that they can provide through reflective practice. Our facilitators are committed to helping our clinicians with their continual professional development.